In this episode:
What is behavioral health? In this season’s inaugural episode, our guests talk with host Dr. Ellen Beckjord about what behavioral health means and share resources to help us get back on track as we move forward from COVID-19.
Have questions? Email us at [email protected]
Resources:
Are you experiencing a crisis or are concerned about a loved one?
For help with addiction, call the Substance Abuse and Mental Health Administration’s hotline at 1-800-662-4357, or click here.
Residents of Allegheny County can call resolve Crisis Network which provides crisis counseling for a variety of issues, at 1-888-796-8226, or click here.
For help with a mental health crisis, reach National Alliance on Mental Illness by dialing 988, or click here.
UPMC Health Plan members can learn more about behavioral health programs, tools, and resources, by clicking here.
To learn more about Community Care Behavioral Health, click here.
Visit the Good Health, Better World podcast page, here, and read the full transcript, below:

Dr. Ellen Beckjord: In this first episode of Good Health, Better World, we’re going to talk about how to lay a foundation for future episodes in our ongoing discussion about behavioral health. And I’m excited to welcome to the first episode Dr. James Schuster, chief medical officer for the UPMC Insurance Services Division and clinical professor of psychiatry at the University of Pittsburgh, and Diane Holder, executive vice president at UPMC and president and CEO of UPMC Health Plan. Diane, welcome to Good Health, Better World.
Diane Holder: Thank you. It’s great to be here.
Dr. Ellen Beckjord: Dr. Schuster, welcome to Good Health, Better World.
Dr. James Schuster: Thank you. Looking forward to it.
Dr. Ellen Beckjord: Really appreciate you both making time to talk with us. And since this is our first episode where we’re going to lay the foundation for behavioral health, I’m going to start with a general question about how you would define behavioral health and ways that we distinguish behavioral health from other terms, kind of in that family, like mental health and behavioral medicine. So, Diane, if I could please start with you: How, in your own words, would you define behavioral health?
Diane Holder: So, behavioral health is a term that emerged over the last couple of decades where people began to look at the component parts that impact people’s thinking, behavior, feelings, mood. And, so, if you look at the classic definition of mental health, those are really more psychological/psychiatric kinds of terms and behaviors.
If you look at substance use, that really has to do with people who are using various kinds of substances that alter mood and behavior. And I think that because those are so often connected — not always, certainly, but they are related in some ways — people began to use the term behavioral health, which was a more global approach to saying, “How do we think about people and their needs for mood behavior and different things that we can do to help support them psychologically, psychiatrically, etc.?” Behavioral medicine is also an interesting term and often gets confused with behavioral health.
Behavioral medicine, I think in its sort of simplest definition, is a way of using behavioral information and knowledge to improve people’s physical health outcomes.
So, for example, if you’re diabetic and we know that part of what you’re struggling with is how you eat, how you exercise, and perhaps your mood is influencing that, it’s hard to exercise, or perhaps you’re not really clear on what behavior techniques are like. Maybe you never knew that keeping a journal would help you with your food. So, these are experts who apply technology that changes behavior in order to improve physical outcomes.
Dr. Ellen Beckjord: I really like that definition and what you’ve said about the distinction between mental and behavioral health.
Dr. Schuster, if I could ask you, how might you think about or define behavioral health, in your own words, or build on what Diane’s just shared with us?
Dr. James Schuster: Yeah, I think Diane did a really nice job of outlining the core concepts. One of the things that I think people often get confused about, actually, is the idea of mental health versus behavioral health.
And as Diane noted, behavioral health really includes many things beyond mental health issues. But often, people use the two synonymously and are, I think, sometimes a little confused about them. So, I think this idea of behavioral health, including many concepts and many ways of thinking about how we feel or how we behave beyond what might be addressed through a term of a mental health disorder, is important.
The other thing that I just wanted to highlight is, often people wonder about, you know, if I have a behavioral health issue, does that mean I have an illness or do I have something that might be defined as an anxiety disorder or depressive disorder?
And I think a good rule of thumb to think about is we all have anxieties, we all have stresses that we work with from day to day. And I think whether or not something is a disorder is often something that really interferes with our function over a period of time.
So, if for several days we can’t sleep well, we’re having trouble thinking and making plans for the day, we’re having trouble going to work — then we might have something that’s more in the realm of a disorder or something for which you might think about treatment at some point. But that’s really a small subset of the issues and themes that we think about as part of behavioral health more broadly.
Dr. Ellen Beckjord: I really think that for a number of reasons, we’re seeing behavioral health get more attention in lots of ways. And I’m excited to talk with both of you about that.
But if I could stay with you for a minute, Dr. Schuster, to put this way of thinking about behavioral health into context — and you’ve started to describe this already — but would you mind giving us a few more examples of behavioral health challenges, and especially how individuals can get support for dealing with and overcoming them?
Dr. James Schuster: One other way of thinking about behavioral health is that it encompasses what we would think of as healthy behaviors.
So, when we’re trying to think about managing stress, anxiety, and you asked about how people can address these things, certainly starting with healthy behaviors is as important for behavioral health issues— things like anxiety and depression — as for things like high blood pressure or managing our weight or other daily challenges that we have.
So healthy behaviors are probably a good place to start. In terms of how people can access services, or particularly if they’re having trouble functioning in some ongoing way due to the things that they think have a behavioral health or a behavioral component, there are many ways that people can really reach out for care, and there’s many studies and much work done now that show that things like regular exercise, regular sleep, not drinking too much alcohol or using other substances, that all those things have really important positive effects on how you feel from a behavioral perspective, as well as a physical one.
There are other ways in which people can get help. Many people find that other resources in their community that they might often access or have connections to are helpful.
So, there are a number of studies that suggest, for example, for people who are religious, that engagement in their church or their synagogue or their mosque is a really helpful way of addressing, of helping them feel supported and helping them feel less stressed. If people are engaged with other community organizations, those are really helpful as well.
And we live in an age now when people tend to be less engaged in their community organizations than folks tended to be maybe 30 or 40 years ago. So, there are also other helpful organizations that are available specifically around behavioral issues.
So, for example, there’s an organization, the National Alliance for Mental Illness, that has many resources available. There are other organizations that have resources people can use, both to help themselves and to learn from other people who are undergoing challenges. And then there are also formal treatments that are available to individuals.
Dr. Ellen Beckjord: A theme that has emerged across the conversations we’ve had this season has been around the existence of treatments and resources for helping people deal with and overcome behavioral health challenges, but sometimes [there are] disconnects or gaps with getting those resources and treatments to people who need them. And Diane, you have been such a champion for health equity, not just in behavioral health, but across the board.
Could you say a little bit about your view related to health equity in the context of behavioral health and what you’re hopeful about, with respect to how we’re making progress?
Diane Holder: Sure. If I think about what causes there to be a lack of health equity, what creates this disparity where some people are able to have health outcomes that are more positive than other people?
And we know, basically, we’re all born with a somewhat different genetic map. We don’t pick our parents. And if you look at the difficulties for people whose lives are complicated by poverty or discrimination or other kinds of problems that are typically not of their own making but are very impactful in their lives, we look at those groups of people and we say they actually, on metrics for health, they’re not doing as well, whether that’s diabetes, whether that’s depression, whether that’s other kinds of conditions, mental health or physical health.
And as we look at, how do we address this? And these problems have been around forever. But these differences, I think they sort of became front and center during the pandemic. And I think the other thing that happened during the pandemic was that the average person found themselves very rapidly going from what had felt like whatever their normal life was, to a whole series of stresses and difficulties that that compounded.
There’s a lot of things that fueled a lot of anxiety, right? And I think in some ways, it gave a bigger heart to the nation to recognize that we all are sometimes victims of circumstances, not of our own making.
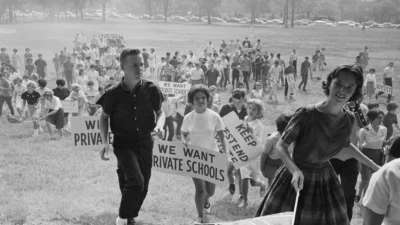
You know, there’s a long tradition in our country that we came out of a very puritan-like culture, right? And there’s been a lot of history of people being blamed for their own problems, and those included the problems of mental health. And, so… there was a little bit in my mind of a consciousness-raising that we are all vulnerable to lots of things, and that sometimes the ways you help people and build back some resilience takes a whole variety of different strategies.
And so, to me, when we start looking at, you know, through the lens of health equity and health disparity, we have to ask ourselves what the drivers are. And I always think that it’s been kind of a classic thought experiment to say, you know, there’s a reason they say, you know, “walk a mile in your shoes” before you understand the world from somebody else’s point of view.
I think that one of the things that was pretty important was the ability to move quickly to telehealth, the ability to get better access for people. And I think it mattered and helped. And the percentage of the use of telehealth for that particular set of disorders or problems was higher than most of the other kinds of problems people had. So, I am a little bit optimistic that we’ve learned, and we’ve learned to recognize that there are some things that we could do that wouldn’t maybe be all that hard to do and that we could improve the conditions for many people.
Dr. Ellen Beckjord: So, one observation and then a question for both of you — both of you really at your core, in part, are behavioral health professionals. And I’m curious about how you’re both thinking about how we can build on the momentum that I do think the pandemic has created around a potential reduction in stigma associated maybe not with behavioral health broadly, but perhaps with vulnerability that lots of us, all of us in many ways, experienced vulnerability during the pandemic, as an equalizer of sorts.
Some people who were already vulnerable, certainly [were] disproportionately affected. But ways that we can build on that, because I don’t know if both of you [have, but] I’ve been thinking about this recently. Do you remember the film “A League of Their Own” with Tom Hanks? Do you remember there was the one player who kept crying and Tom Hanks would get really mad at her for crying. And then one day, she didn’t cry and he held it together, but he was sort of shaking.
He was so frustrated. That’s how I have felt, like, “Oh, behavioral health is important.” And you’re like, “Yes, some of us have known that for a long time!”
But now it really is, in many ways, front and center. So, there are so many ways that, within the Insurance Services Division, we address behavioral health and integrate it into everything we do.
But I would love to hear from both of you about the things we’re doing in the Insurance Services Division that you think really have positioned us to capitalize on this momentum to meet this moment.
And Diane, I’ll start with you, and then Dr. Schuster would love to hear from you.
Diane Holder: I think one of the things that we’ve done at the UPMC Health Plan Insurance Services Division is that we’ve tried to build a culture of whole-person care and thinking.
So, I think part of what we need to overcome, in many ways, is that the way that medicine at large has been organized, historically, has been very much focused on acute care. It’s been focused a lot on procedures; it’s been focused a lot on, really, specialization.
And that, over time, I think professionals were trained and grew up in silos. And I think that it’s been an opportunity over the past many years to try to say, “What can various disciplines and training come to the table together, to think about differently, and how would you apply more holistic thinking to whatever problem you’re trying to help people with?”
So, in my mind, you know, the opportunity for looking at the full spectrum of needs that people have — there’s nobody without physical health needs. And there’s nobody without mental health, behavioral health needs, quite honestly.
I mean, that’s who we are. We’re human beings that have a whole spectrum of conditions, problems, issues, opportunities, strengths. Right?
And, so, bringing together people who can conceptualize that and say, you know, ‘How does this piece influence that piece? How does my ability to learn and thrive and grow get influenced by my level of social support, the kind of access I have to high quality air and good food, and the kinds of things that we know really make a difference in people’s lives?’
You don’t have to have a penthouse. What you have to have, essentially, is a safe roof over your head. There’s a reason that Maslow’s hierarchy exists. You’ve got to have basic fundamentals met before you can do much more.
And I think one of the things that’s been really exciting for us to be able to work on over the years, at the Insurance Services Division, is trying to understand, yes, we believe very strongly in best practices in any kind of medical or clinical care, but we also know that clinical care unto itself is not what drives health outcomes.
What drives health outcomes, in my opinion, is yes, it’s really important to have access to good clinical care, but it’s really important also to have access to all the other things that surround you.
And that’s why we work a lot on things that people call the social determinants, the social influencers, and help to focus on those things. Because one of the things that we know — and there’s a very strong literature [on this] — is that stress is one of the leading causes of illness. And stress, quite honestly, is a killer.
So, one of the things I think we try to do, looking at health more holistically, is think about all the ways that you have to support a person holistically. And that isn’t going to come from the medical community, per se. It’s going to be a partner to the medical community, I hope.
Dr. Ellen Beckjord: And not directly, but implicitly — and maybe this is because we’ve had conversations where I’ve heard you talk about constructs like resilience, the importance of resilience implicitly — in that I hear a strengths-based approach, which I think is part of our whole-person approach in the Insurance Services Division, not to discount the challenges that people face. But I think we have a strengths-based approach to how we serve our membership.
And I think we have a strengths-based approach to how we think about our internal function and operations, our drive to continuously improve, critically evaluate, iterate, and do better.
Diane Holder: Yes, I believe that strongly. It’s almost impossible to improve if you have nothing to build on. And I think there’s always something to build on. And I think the opportunity to harness strengths and be able to support and layer is critically important.
But the most important thing I think about strengths-based is, it’s hope-inducing — and nothing gets done without hope.
Dr. Ellen Beckjord: Well said. Dr. Schuster, I would love to hear from you on this topic. And I’ll also mention that in an upcoming episode in this season, we hear from Dr. Matt Hurford, who is currently president of Community Care Behavioral Health, and Dr. Geoff Newmark, who is chief medical officer at Community Care Behavioral Health.
Of course, Community Care Behavioral Health is part of our organization. You have both led that organization, so we’d love to hear from you, Dr. Schuster, about how Community Care Behavioral Health fits into our spectrum of approaches and services related to behavioral health. And anything else you’d like to add?
Dr. James Schuster: So, Community Care has really been part of the Pennsylvania Medicaid Behavioral Health Program known as Behavioral HealthChoices.
And it’s really a wonderfully designed program that really tries to address these issues of community and support for individuals. It’s a very interesting model in which the county behavioral health leadership in each Pennsylvania county actually has a role to play in overseeing the program and managing it.
And all the counties partner with a managed care organization like Community Care to affect and implement the program. Community Care has been very fortunate.
After Diane’s founding back in the mid-’90s, it grew dramatically and now works for 43 of the 67 counties in the state. And it’s really a wonderful experience in which there’s a strong focus on public health issues, both driven by the county as well as by the state, as clear outcomes for the program. So, there’s been lots of extensive focus on things like creating peer support services for members, case management services to help people address things like housing and food security, and other resources that are such an important part of the whole health picture that Diane was referencing.
You know, several years ago, Hillary Clinton wrote a book about how it takes a village to raise a child. And I think one of the things that became clear in the pandemic was that this village concept is important for each one of us.
And, you know, you asked how we could continue to build on that theme and that feeling that people tended to have, or that became more evident during the pandemic. And I don’t think there is one simple answer to it, but I do think that changes in payment systems have actually helped to highlight that actually for health practitioners, because health practitioners are now being paid, to some significant degree, often for the outcomes of individuals from their treatments.
And the outcomes are often as or more dependent on behaviors of the individual as they are in the specific treatment that they receive. So, if someone has surgery, their recovery is often dependent to some degree both on their underlying physical state — so, whether or not they’ve been exercising, had good nutrition, stopped smoking and so on before the surgery — as well as those behaviors after the surgery. So, the payment models actually made these themes of underlying behaviors and what we talked about as behavioral medicine much higher in the consciousness of many medical practitioners. So, I think that’s one thing that’s been really helpful.
One of the other things that we found is that it’s also possible — and we actually discover this, I think, most dramatically in some of the work at Community Care Behavioral Health — where we actually worked with practitioners, mental health practitioners to help them understand these behavioral needs and challenges of the people they worked with. So, we did lots of training and incentives for them to focus on these behaviors. Things like exercise, regularly following up with their primary care physician, eating habits, and other daily activities that really impact people’s underlying physical health problems.
What we found over time, actually in a very structured, federally-funded study, was that those interventions really help people’s physical health outcomes. That even within a period of a couple of years, they had less hospitalizations. They saw their primary care practitioner more often and they were more likely to take medications that were prescribed for conditions that were important to their health.
And we also found, even, that these behaviors actually help their behavioral health conditions as well.
Dr. Ellen Beckjord: One of the things that I think is particularly exciting and hope-inducing about behavioral health [is] there’s really opportunity to leverage improvements at so many different levels, whether it’s at the individual level, the community level, the level of the care delivery system and the policy level.
There are ways that we are making advancements in behavioral health across all those levels and continue to do so. But I would like to give each of you an opportunity — and Dr. Schuster, if it’s OK, I’ll start with you, to highlight one or two things that you feel particularly hopeful about or excited about with respect to impact on improving behavioral health potentially at a population level.
Dr. James Schuster: Well, certainly one area that we’ve focused extensively on, and had I think some great success with is, really trying to address the opioid crisis across the counties in Pennsylvania, the regions that we work in, which now for the insurance division really includes all of Pennsylvania.
We’ve worked really intensively with our own pharmacy team and with providers, pharmacy teams and the prescribers particularly, but not only primary care physicians to really reduce the prescribing of opioids and the number of opioid medications prescribed has declined by over half. And in some areas greater than that, for some populations, much greater than that over the last five or six years. So, there’s been a really dramatic decline in that, while we’ve continued to work and try to address other ways to manage pain for people.
At the same time, we’ve done extensive work to try to increase access to treatment for individuals who do have problems with opioid dependency.
The other area that I’d like to highlight is that there’s been very significant growth in peer support services, both for people with mental health challenges and for people with substance use challenges.
Most counties 10 years ago didn’t have peer services for either behavioral health, for either mental health or substance use conditions. And now almost all the counties have those individuals in place.
Dr. Ellen Beckjord: Those are two great examples. I’m so glad that you brought both of those up. Thank you. Diane?
Diane Holder: So, when I think about what makes me optimistic and as you look to the future, I sort of find myself looking backward and potentially forward at the same time.
And when I look backward, I recall the era where we were talking a lot about biopsychosocial as a model that’s going back at least 30 years. And we said, you know, those are all important elements of what’s going to actually make an impact for people in terms of their mental health condition. And when I look to the future and fast forward over several decades, I think we have made progress in all three areas.
And I think that we’re on the brink, I hope, of the sort of the great beyond where the brain has been like outer space, right? We know less about the brain than about any other organ and the mapping that’s occurring and the ability for imaging and the kinds of things that we think might allow us to have different kinds of pharmacological interventions, different kinds of treatments that will be innovative.
I mean, there’s just a lot of opportunity at that very core biological level that will be very important in addressing some of the profoundly serious conditions that we see.
But we also know that in [addition] to biopsychosocial, we’ve learned a lot more about the impact of social relationships on mood and other kinds of mental health issues.
We know a lot about social isolation and why that’s so hard and how, when you’re building resiliency, the importance of social support for people to function well.
And then as we’ve been emerging, and I think this has been more the conversation that’s been raised lately is that whole social impact, you know, what is that “surround-sound” that’s happening all the time in people’s lives and how do you influence those pieces and how do you bring parts of the community together that are both clinical and social and other kinds of supports that together will have impact?
So, when I go back, I think we had sort of the right concept a long time ago. We just actually didn’t put it together as well and we’re not there. But I do think that people see the importance of all and that it’s not an either or.
Dr. Ellen Beckjord: I think that’s a good representation of where we are in many ways and in that way it’s an exciting time.
Diane, is there anything else you’d like to add or circle back on or that comes to mind?
Diane Holder: Well, part of what we’re living in right now, in a sort of virtual digital world, especially with adolescents, is having a lot of impact on mental health issues and social contagion problems.
But the context for the world people are living in is changing, has changed rather dramatically. And that’s something I think we need to give attention to and know where the risks are associated with that, but also know where the potential opportunities are with that.
Dr. Ellen Beckjord: Let’s build on that for just a minute, because I really like the way you described that. There is enormous potential to leverage connectivity, to promote connection, and there are lots of examples where that happens.
Diane Holder: So, I think the opportunities that we have related to the connectivity in the world are really quite profound.
One of the rate-limiting factors in people accessing health care is this supply difference, right, between what are the kinds of things people are seeking and looking for and what’s available to them. And that mismatch occurs in many, many ways. I think one of the things that we’re learning — at least I’m learning, I’ve been learning, I hope — is that your health is heavily in your own hands and that you will, hopefully, get guidance and support from the people in your lives and certainly a primary care doctor or a mental health professional of some sort.
I think the sense of agency is so critically important. And it would be something that I think, in many ways, you’re seeing young people be able to exert in a different way than perhaps they did in earlier generations.
The capacity to connect, learn, be exposed has risks, of course, but it also has tremendous opportunity. The ability to take your own needs into your own hands and say, “Gosh, you know, I was just diagnosed with this condition. Well, what can I learn about it?” You can seek guidance and support in different ways. And you can, I think, open your world differently.
And, so, I think one of the real potentials is for us as health plans and health delivery systems to sort of harness that and understand that one of the ways we can meet people where they’re at differently is to actually try to figure out what that is, instead of us superimposing upon them how we think their needs should be met.
Dr. Ellen Beckjord: My sense — [and] feel free to disagree — is that over the last 10, 15, 20 years, there has been this sort of emergence of a recognition of the critical importance that social factors play in health. And then, after that recognition, it felt to me like it almost became a hot potato once it was recognized that these social factors played a critical role in health. And I’m talking about social influencers of health, which our whole first season of Good Health, Better World focused on.
It then became apparent no one was really sure who would step in to deal with that and what that could look like. And here at UPMC Health Plan, it feels like we took that head-on with our Center for Social Impact a couple of years ago.
But the way that it seems to me we’ve taken it on is, again, back to this kind of coordinating, navigating function. There are lots of social services out there, but they exist in a completely disintermediated and highly complex web that makes the healthcare system look like a walk in the park in some ways.
And so much of what we’re doing at the Health Plan is helping people navigate those services, providing a very high level of service to help people access and onboard into those services. I would love to hear — feel free, of course, to disagree with any of that. But your take on that part of the social component of biopsychosocial and how it’s relevant to behavioral health.
Diane Holder: I think it’s extremely relevant. I mean, from my vantage point and maybe it’s, you know, in part based on, I trained in social work and public health and it never occurred to me that you wouldn’t look at the context of somebody’s condition, their life, when you were trying to figure out what needed to happen.
And I quite honestly think that that part of what has made it harder to get from here to there over time is that we evolved increasingly as a national health care delivery model for increasing specialization so that there’s pretty much a body part doctor for every body part you have, right?
And you can look at our population, our members that we serve. And if you pull up the data in terms of the numbers of medications that some of the people who are quite ill or complicated, the number of physicians, I mean, you can see people have seen 10 doctors and are on 15 medications.
And there is really very little in the traditional system of care that helps you connect those dots. If you then say, add to that all of the component parts. So, in addition to just managing medications or managing a variety of conditions and illnesses that people have and without much of a quarterbacking function, and then you say, well, what if you add to that the layer that this person has unstable housing, this person has food insecurity, this person’s actually hard for them to actually manage to get through school or hold a job or do these various kinds of things that their functioning is not optimal, right? How do you begin to connect all those pieces?
And I get back from my point of view to, there’s a navigation function that’s extremely valuable. There has to be some methodology by which you figure out the prioritization of those things and how you’re going to help people basically move toward a capacity to be something in a more self-sustaining fashion.
I don’t think this function is out there easily outside of health plans, quite honestly, that can see the map — and then not only see the map but have an advocacy attitude because it’s not good enough to say, “Here, call this place, they’ll help you.”
What’s important is helping people understand what the barriers are to even getting that help or getting that support or making use of it in a useful way.
But I think it’s through the attitude of advocacy and a whole-person thinking that by putting those functions together, you then can map out partnerships between one part of a system and the next part of a system, because everybody has to do their piece or you’re not going to be able to do it. And I think that’s what the Center for Social Impact concretized for us.
Dr. Ellen Beckjord: Very well said.
I want to thank both of you so much for spending time with us to lay the foundation for behavioral health. We’re very excited about this season of Good Health, Better World. So, Diane, thank you so much. Dr. Schuster, thank you so much. It’s been just wonderful to talk with you today.
Diane Holder: Well, thank you. This was fun.
Dr. James Schuster: Yeah, it’s been great to participate. Thank you for inviting us.
To listen to the show, click here.